authors: Walter Tsang MD
updated: 8-1-2018
A review of effective treatment options for cancer-related palliative care.
What is palliative care?
Palliative care is a form of medical care that is focused on providing relief from the symptoms of a serious illness.
A serious illness, such as cancer, creates many stressful and uncomfortable symptoms (nausea, fatigue, anxiety). These symptoms may be caused by the biological progression of the disease or they may be the side effects of the treatment.
Palliative care seeks to improve the quality of life for the patient and the patient’s family by providing relief from the symptoms of an illness and the side effects of treatment.
An integrative approach to palliative care includes both conventional and alternative treatment options.
- Conventional therapy includes: prescription drugs, pain-killers, etc.
- Alternative therapy includes: herbal supplements, vitamins, diet, cognitive behavioral therapy, etc.
It makes sense to be open to the best possible palliative care. Often, the best treatment includes a combination of both conventional and alternative therapy. Below, we summarize the most effective integrative approaches to common symptoms experienced by patients struggling with a serious illness.
Click on a symptom below to learn about effective treatment options.
The symptoms listed above are commonly experienced by cancer patients. However, the symptoms discussed on this page are not unique to cancer patients. For that reason, this page serves as a resource for people managing other serious health concerns (diabetes, heart disease, COPD, dementia, ext.)
Walter Tsang MD is a medical oncologist in Banning, California. Dr. Tsang treats cancer patients at Redlands Community Hospital.
This article is intended to be used as a general educational resource. Please consult with your physician in regards to the best treatment for your particular medical situation.
Depression
Being sick can be incredibly depressing. Hearing bad news regarding your own body is depressing. Spending weeks or months in a hospital can also be depressing. Racking up costly medical bills is also….you guessed it…depressing.
For all these reasons, cancer patients are 4 times more likely to be depressed than the general population.
Depression is more than just a brief feeling sadness. Depression is a persistent low mood that prevents you from engaging in the world in a positive way.
Similar to anxiety, depression is often a natural response to the reality of dealing with a serious illness. However, patients cannot lets this emotional disorder take control of their lives. You need to be pro-active.
Judith Carlin, Wikimedia Commons
Painting captures the inescapable feeling of depression.
How do we treat depression in palliative care?
The standard treatment for depression is some combination of psychological therapy and anti-depressant drugs.
Anti-depressants
The most common prescription anti-depressants are Selective Serotonin Re-uptake Inhibitors (SSRIs) and Serotonin Nor-epinephrine Re-uptake Inhibitors (SNRI). These drugs work by raising serotonin and nor-epinephrine levels in our brains. Popular brands include: Zoloft, Prozac, Paxil, Celexa and Cymbalta. SSRIs and SNRIs are effective for some patients, but certainly not for everyone. Its difficult to give an exact number for the success rate (efficacy) of these drugs because each published report is different. From everything I’ve read, I think a fair approximation is 50% efficacy. About half the people on anti-depressants report improvements.
Alternative approach to treating depression
Some of the more popular natural products used to combat depression include: St. John’s wort, SAMe, valerian and rhodiola.
SAMe is an abbreviation for S-Adenosyl-L-methionine. This is a chemical found naturally in the body. SAMe is made in the body from methionine, an amino acid found in many proteins. It is known to help many of our cells function normally. Scientists observed that people suffering from depression also had abnormal levels of SAMe. This led to the idea that depression could be reduced by supplementation with SAMe capsules. Unfortunately, it is not clear whether this supplement is significantly helpful for depression. About 40 studies have been performed. Some of them did show improvements in regards to the severity of depression. However, these trials need to be repeated with larger sample sizes and they need to be conducted for longer periods of time.
St. John’s Wort is a small herb with yellow flowers that is routinely used to treat depression. Many studies show that St. John’s wort works as well as traditional antidepressants for the treatment of mild-to-moderate depression. Interestingly, St. John’s wort also has fewer side effects than most antidepressants. However, it should be noted that St. John’s wort can react poorly with certain chemotherapy drugs and birth control drugs. If you’re currently on other medications, then consult with a physician before using this plant.
Valerian, ginkgo, rhodiola and saffron are additional plant-based supplements used to combat depression. However, in our opinion, there is insufficient evidence to support the claim that these approaches are effective.
5-HTP, a serotonin precursor molecule, is also used to alleviate depression. Although, we are also not aware of any large studies performed to verify the effectiveness of 5-HTP for depression.
Therapy methods used to combat depression
Depression is a very personal and emotional condition. Each person has their own struggle and each person is walking around with their own unique brain. Everyone has to work through their issues in their own way. Drugs or herbs are not always the answer.
Below we list some of the most effective psychological methods in regards to relieving depression.
- One-on-one psychological therapy – classic psychotherapy, delivered over 6-8 weeks, patients often prefer this method
- Cognitive behavioral therapy – seeks to identify and re-structure the thought/action patterns that cause emotional distress
- Interpersonal therapy – focuses on the patient’s personal relationships and interactions with other people
- Dignity therapy – aims to strengthen a patient’s sense of meaning and purpose at the end of life, reduces existential crisis
- Mindfulness-based therapy – uses meditation, breathing techniques and yoga to help patients focus on their thoughts and feelings
Return to our main list of symptoms.
Fatigue
Fatigue is a persistent feeling of physical, mental or emotional exhaustion. This is different than simply being tired. In general, fatigue does not go away even after a good night’s sleep.
Fatigue is a very common symptom among cancer patients. Both cancer and the treatment for cancer can cause fatigue. According to one study, fatigue occurs in 80% of patients treated with chemotherapy and 90% of patients receiving radiation therapy.
It’s not clear what is happening in our body when we becomes fatigued. Possible explanations include: mis-regulation of our HPA axis (hypothalamus-pituitary-adrenal), depletion of our serotonin levels or mis-regulation of cytokines in our body. Cytokines are the communication signals used by our immune system.
The face of fatigue.
Integrative approach to treat fatigue
Ideally, you want to identify the source of your fatigue and then eliminate that source.
That said, finding the root cause can of fatigue can be a real challenge. Part of the problem is that fatigue is usually multi-factorial. This means that fatigue is often caused by many different factors. Infection, insomnia, anemia, chemotherapy, radiation, depression, organ dysfunction and chronic pain are all contributing factors. This multi-factorial aspect is part of the reason conventional medicine has a tough time treating fatigue.
Talk to your physician about which habits or health issues may be contributing to your fatigue. For example, we know that anemia can cause fatigue. If you think anemia might be causing your fatigue, you’ll want to focus your diet on foods that are rich in iron and vitamins.
Prescription drugs used for fatigue
Most of the prescription drugs used to treat fatigue are some sort of stimulant. Conventional fatigue drugs include methylphenidate (Ritalin), modafinil (Provigil), pemoline and donazepil. Modafinil, for example, is a classic stimulant. This drug acts by inhibiting GABA signals in our brain and activating our excitatory neurotransmitters (serotonin, dopamine and nor-epinephrine).
Many people who experience fatigue are also depressed. Interestingly, some people find that a low dose of an anti-depressant can improve their sleep and also reduce fatigue. Bupropion is an example of an anti-depressant that’s studied for its ability to treat fatigue. Inflammation can also contribute to fatigue. For this reason, treatment with an anti-inflammatory drug, such as dexamethasone, has also shown the ability to reduce fatigue.
Lifestyle changes to address fatigue
A healthy diet can dramatically improve daily energy levels. Heath care professionals often suggest avoiding sweets (refined sugars) as this high-sugar type of food can lead to energy crashes throughout the day. A low-carbohydrate diet that’s rich in fruits and vegetables is strongly recommended. For reference, here is a thorough list of nutrient-dense foods. These foods deliver many of the vitamins, minerals, fiber and protein we need in our diet. Many physicians also recommend adding probiotics to your diet. A healthy gut microbiome appears to be linked to energy levels and fatigue.
Drinking coffee is fine and often necessary for many people to fully wake up. But, make sure you don’t over do it. Try to stop drinking coffee at noon. You don’t want caffeine to interfere with your 8 hours of sleep.
Speaking of sleep, you really need to get those 8 hours of sleep. I realize this is a challenge for many people, but it is so critical. If you’re a light sleeper, try earplugs and white noise. I’ve found the sound of rain at low volume (from my phone speaker) helps keep me in a deep sleep. When all else fails, you can try a supplement or pharmaceutical. Melatonin, valerian and ambien are some of the more common sleeping aids.
Exercise seems to be one of the best non-chemical treatments for fatigue. Even if you’re exhausted, try to fit some cardio workout in at least 3-5 times week. This doesn’t have to involve going to the gym. Fast walking around the neighborhood or office can do the job. When you burn off energy during the day, you increase your chances of getting a good night’s sleep.
Psychological factors also contribute to fatigue. Feeling poorly about yourself is exhausting. Feeling helpless is exhausting. Feeling like your life is spiraling out of control is exhausting. Talking with a counselor or therapist can help you figure out strategies to work around or resolve these psychological issues. Cognitive behavioral therapy and Self-management strategies are two techniques that are specifically effective at treating fatigue..
Medicinal plants used to address fatigue
Over the past few decades, physicians have seen increasing interest in the clinical use of medicinal plants to relieve fatigue and cancer-related fatigue. The following natural products have demonstrated effectiveness in treating fatigue:
Ginseng, specifically American Ginseng, is an ancient Chinese herb used to treat fatigue. For reference, here is a clinical trial, performed with 364 patients, that determined ginseng (Panax quinquefolius) could improve cancer-related fatigue over an 8 week period.
Rhodiola is a succulent plant that grows along mountain ranges in Europe and Asia. Historically, people have used this plant to address depression, anxiety and fatigue. Today, Rhodiola is commonly used to improve energy levels throughout the day and help the body adjust to stress. Many clinical trials have been performed on Rhodiola and there is evidence this plant can help ease stress related fatigue. Here you can read our full report on Rhodiola.
Below, we list additional supplements often used to reduce fatigue. Please click on each item to read the supporting scientific document.
Return to our main list of symptoms.
Weak immune system
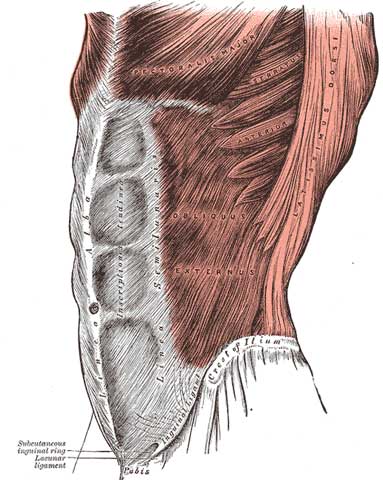
Our immune system includes our skin, spleen, lymph nodes, bone marrow and our white blood cells (neutrophils, leukocytes, ext.)
We rely on our immune system to fight off infections caused by bacteria, fungi and viruses. We want all components of our immune system working to battle an infection.
Unfortunately, a weakened immune system is one of the common symptoms of a serious illness. For this reason, patients in palliative care are often more vulnerable to infections.
People that are experiencing chemotherapy, transplants, auto-immune disease, neutropenia or radiation often do not have the full power of their immune system. They are at risk of an infection taking hold in their body. These folks will want to do everything possible to boost their weakened immune system.
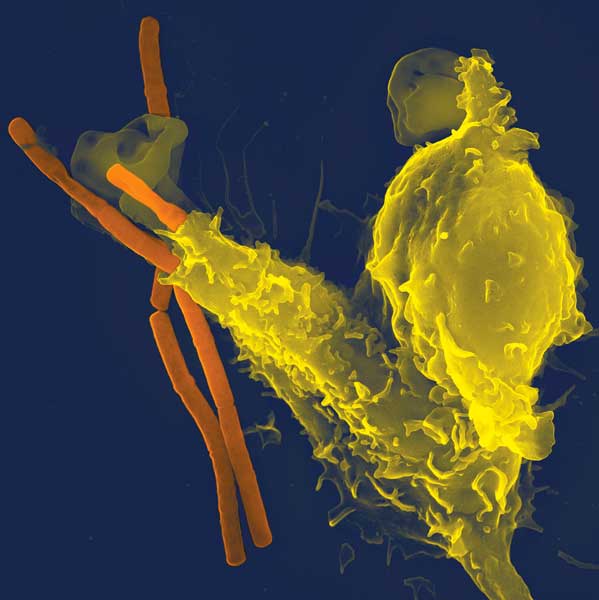
Volker Brinkmann, via Wikimedia Commons
Our immune system at work.
A neutrophil (yellow) is seen attacking bacteria (red)
How do you strengthen your immune system to help prevent infections?
First of all, you can follow some basic rules.
- Get lots of restful sleep
- Avoid cigarettes
- Exercise regularly (commit to some high-energy movement every day)
- If you drink alcohol, drink moderately
- Avoid germs (wash hands, keep your distance from sick people, cook meats thoroughly)
- Eat a diet high in nutrient-dense fruits, vegetables, whole grains and healthy meats. Here’s our list of recommend foods.
Focus on vitamins that support the immune system
Vitamin C should be consumed every day because our body doesn’t naturally produce or store it. We need vitamin C for many cellular processes vital to our health. Fortunately, many foods contain this immune-boosting vitamin: oranges, bell peppers, spinach, kale, broccoli, tangerines, mango, strawberries, Brussels sprouts, tomatoes, snow peas, papaya, kiwi and melons.
Beta-carotene is a natural pigment molecule in plants (beta-carotene creates the orange color in carrots). When we eat beta-carotene, our body converts this molecule into Vitamin A. Foods that contain beta-carotene and other carotenoid molecules include: beets, carrots, corn, asparagus, collard greens, kale, green peppers, broccoli, pumpkin, squash and apricots.
Vitamin E helps the body fight infections and acts as a powerful antioxidant. Foods that include vitamin E include: broccoli, avocado, chard, papaya, spinach, sunflower seeds, mixed nuts and mango.
Vitamin B6 is required for many of the biochemical reactions required in our immune system. Vitamin B6 rich foods include salmon, tuna, chicken, dark-leafy vegetables and chick peas (hummus).
Zinc and selenium are minerals that also act as antioxidants and should be a part of a balanced diet. Zinc can be found in oysters, red meat, nuts, whole grains and chicken. Selenium is found in Brazil nuts, beef, whole grains and poultry.
Herbal supplements that help enhance our immune system
Certain plants and mushrooms have demonstrated the ability to boost our immune system.
Turkey Tail mushroom has been consumed since the 15th century in China during the Ming Dynasty. This fungus contains two powerful polysaccharides. These compounds are being researched as part of a $5.4 million collaboration between Bastyr University and the University of Washington. Research is exploring whether turkey tail can improve immune function in women with stage I to III breast cancer.
If you are looking for Turkey Tail, I recommend Turkey Tail Capsules from Host Defense. Host Defense has an excellent reputation in the supplement industry.
Black elderberry is a tree native to most of Europe. Syrup made from the berries of this tree can benefit our immune system via slowing down virus activity, enhancing our cytokine levels and boosting antioxidants in our body. Here you can read our full report on black elderberry.
Echinacea is a purple flowering plant that is native to the Great Plains region of North America. Extracts from this herb are routinely taken to reduce the intensity of cold or flu symptoms. Here you can read our full report on echinacea.
Chaga mushrooms grow on the sides of birch trees in cold, northern forests (Canada, Maine, Alaska, Siberia, ext.) Scientific papers demonstrate the ability of chaga to support our immune cells and serve as a potent antioxidant. Here you can read our full report on chaga mushrooms.
Important final note about the immune system: Once a dangerous infection (bacteria, virus, ext.) has begun to multiply in your body, you will want to kill off this infection immediately. Its time to bring out the big guns. Antibiotics, antiviral or antifungal medications are often necessary at this point.
Return to our main list of symptoms.
Cognitive decline
Brain function can diminish as a result of cancer, chemotherapy treatment, early stage Alzheimer’s or simply as a result of the natural aging process. A decline in cognition includes the following symptoms:
- lack of concentration
- difficulty remembering things
- slower thinking speed
- mental fog
Poor brain function caused by high doses of chemotherapy is known as ‘chemo-brain’. Immuno-therapy treatments can also trigger cognitive impairment. In fact, approximately 56% of palliative care patients experience some form of cognitive decline.
In addition, a diagnosis of cognitive decline is also bad news for the caretaker of the patient. Anxiety tends to be very common among caretakers in charge of loved ones diagnosed with dementia, delirium or cognitive impairment.
Wellcome Images, Wikimedia Commons
An 1892 sketch of a man with advanced cognitive decline.
Treating cognitive decline
Currently, there are no FDA approved drugs to treat mild cognitive impairment. Scientists are aware of several genes that correlate with the onset of Alzheimer’s (apoE4, Aβ42, tau) but we still do not fully understand the cellular mechanisms that cause the disease. However, a series of drugs named cholinesterase inhibitors have been approved to treat symptoms of Alzheimer’s disease and dementia. These drugs increase the amount of acetylcholine in our brain. Acetylcholine is a naturally occurring messenger chemical that is involved with memory and judgment.
Various herbal and dietary supplements are also thought to limit cognitive decline.
B vitamins are involved in the production of several neurotransmitters in our brain. Specifically, vitamin B12 helps keep our nerve cells and brain functioning properly. A deficiency in this vitamin can lead to nerve problems, dementia, poor memory and cognitive decline. In the case of dementia, we know that vitamin B12 specifically lowers levels of homocysteine levels in the blood. Homocysteine is a modified amino acid that accumulates in the blood of dementia patients.
Vitamin B12 occurs naturally in most animal meats and eggs, although not in plant based foods. Due to this discrepancy, vegetarians often develop deficiencies in vitamin B12. This is why its important to remember that nutritional yeast has high amounts of B12. Most vegetarians are not adverse to sprinkling a little yeast on their salads
Ginkgo biloba has been discussed as a medicinal plant that is effective in reducing the development of dementia and Alzheimer’s disease. However, this plant was found to be ineffective in a large, 3,000 patient clinical study published in the Journal of the American Medical Association
Phosphatidylserine is a naturally occurring substance in the brain. Studies suggest that phosphatidylserine supplementation can increase levels of certain brain chemicals that are involved with attention, language skills and memory in aging people with declining thinking skills. In addition, one report shows phosphatidylserine can improve some of the symptoms of Alzheimer’s disease after 6-12 weeks of treatment. Phosphatidylserine treatment seems to be most effective in people with less severe Alzheimer symptoms.
Grape seeds contain a group of chemicals called polyphenols. These polyphenols (GPSE) are currently being explored for their role in preventing neurodegenerative disorders. These grape seed chemicals seem to interfere with the generation of tau proteins in our neurons. But why do we care about interfering with tau proteins? Well, it turns out that many neurodegenerative disorders, most notably Alzheimer’s disease, are correlated with the build-up of tau proteins in our brain cells. If chemicals in grape seeds can disrupt the accumulation of tau proteins in our brain, then that would be a very big deal in the Alzheimer’s research community.
Omega-3 fatty acids are important for the synaptic proteins in our brain. As we age, we want to make sure that our brain has all the raw materials it needs to build neuronal architecture and also to transmit signals across these neuronal highways. Omega-3s (DHA in particular) are among the more important lipid structures in the brain. These polyunsaturated fatty acids lead to higher synaptic transmission and less oxidative stress. Flaxseed oil and fish (salmon, sardines, mackerel and cod liver) all contain high amounts of omega-3 fatty acids. This paper does a nice job illustrating how the use of omega-3s benefits seniors with mild cognitive impairment.
The MIND diet is a relatively new diet that has gained a lot of respect lately. The objective of the diet is to promote a healthy diet and to lower the risk of neuro-degenerative disease, such as Alzheimer’s. Those are lofty goals for a diet, but apparently the diet meets these goals. A large NIH funded clinical study tested these objectives and found that the MIND diet was good to its word.
The MIND diet was developed by a nutritional epidemiologist at Rush University named Martha Morris. Martha wanted to put together a diet that consisted of only ‘brain healthy’ foods. With funding by the National Institute of Aging, Martha and her team conducted a decade long study of her MIND diet on 923 seniors. The results showed this diet could lower the risk of Alzheimer’s disease by 53%. In fact, 35% of the seniors who only followed the diet moderately well also saw a significant reduction in cognitive decline.
The MIND diet is not that difficult to follow. This article describes the components of the diet.
In addition to diets and supplementation, some studies suggest the following lifestyle strategies are also helpful for those dealing with cognitive decline or mild cognitive impairment.
- Regular exercise benefits your heart and the blood vessels that nourish your brain.
- Minimize cardiovascular risk factors. Protect your heart and your heart will support your brain function.
- Remain mentally stimulated and socially engaged. Keep flexing your brain muscle!
Return to our main list of symptoms.
Loss of appetite
Appetite loss is common among elderly adults and cancer patients. When you are battling an illness, your body will often be resting or immobile. In this scenario, its normal for a person to want and need less food. In addition, some prescribed medications such as antibiotics, opiod pain-killers and chemotherapy drugs often further contribute to a loss of appetite.
Early satiety also contributes to appetite loss in cancer patients. In this situation, a person will want to eat a full meal but they can only take in small amounts of food because their stomach already feels full. This false sense of fullness is not fully understood but we do know that regulation of leptin is involved. Leptin is the chemical signal in our body that communicates when our stomach is full.
Dysgeusia is another reason for appetite loss among patients. This hard-to-pronounce word means there are abnormalities in our sense of taste. In fact, more than half of patients treated for cancer report that food tastes different. Your desire to eat food will definitely change if your taste buds are acting funny.
Here are some simple ways to encourage eating during palliative care:
- Eat frequent, small meals. This is easier than 1 large meal.
- Cook your favorite meals with family and friends.
- Exercise lightly during the day.
- Try drinking high protein drinks.
Some people report the following botanical supplements have helped them regain their appetite: Centuary, Blessed thistle and Gentian. We are not aware of any scientific literature supporting the use of these plants to increase appetite.
There is one phase II study showing the ability of Astragali Radix to help cancer patients regain their appetite. Astragali Radix is the woody root of the Astragalus plant (Astragalus membranaceus). This plant has been used in Traditional Chinese Medicine for thousands of years. It’s considered a potent ‘Chi tonic herb’.
Return to our main list of symptoms.
Nausea
Nausea is defined as a feeling of sickness in the stomach that is often accompanied with an urge to vomit.
Both nausea and vomiting are common symptoms that affect the majority of patients dealing with advanced cancer and other serious illnesses. Unfortunately, nausea is a complicated biological symptom and is not fully understood by scientists. Palliative care doctors generally attempt to find the exact source of nausea and treat it with an anti-nausea drug, also known as an anti-emetic.
Common prescription drugs for nausea and vomiting include: dopamine antagonists, selective serotonin receptor antagonists and anti-histamines. In theory, these drugs block the neurotransmitters that are active in the biological pathway that generates the nausea. Unfortunately, the success of these treatments is limited. Many patients using these drugs are over 65 and don’t respond well to the treatment.
A nauseous man depicted in a 17th century Italian oil painting.
Integrative approach to nausea
Ginger and relaxation techniques are two common non-prescription drug approaches to nausea.
Ginger is a tropical plant from southeast Asia. The roots of this plant can spice up a stir-fry and deliver medicinal properties. Ginger is often used to address post-surgery nausea, motion sickness and nausea induced by chemotherapy and pregnancy. Multiple clinical trials have demonstrated that taking between 1-2 grams of ginger before surgery can reduce nausea and vomiting during the day after surgery. Another study suggests that taking ginger before anti-retroviral treatments could reduce nausea and vomiting in HIV patients.
Relaxation techniques are another non-traditional approach to managing nausea. The goal of all relaxation techniques is to induce or enhance the body’s own natural relaxation response. This response includes slower breathing, lower blood pressure and an increase in the overall feeling of well-being. There are various forms of relaxation technique. In terms of nausea, research suggests two relaxation techniques are especially helpful: guided imagery and progressive muscle relaxation.
Return to our main list of symptoms.
Anxiety
Anxiety is a complex human behavior. It is a behavioral response to a threat. When you’re anxious, you activate your HPA axis (hypothalamus-pituitary-adrenal gland). This HPA activation leads to the flight or fight response that often saves you from the dangerous situation.
Sometimes anxiety is the appropriate response. If there’s a real and dangerous threat to your life, then you should be anxious. In palliative care, anxiety is often justified. If you’re dealing with a life-threatening disease and looking at the high probability of approaching death, then it makes a whole lot of sense to be anxious. Death is the huge unknown and that is terrifying to most people.
However, if you’re constantly anxious about threats that are greatly exaggerated in your mind, then anxiety can be very unhealthy. Chronic anxiety places a lot of unnecessary stress on your body and your brain. Many patients dealing with a moderate and manageable illness may still be experiencing high and unnecessary levels of anxiety. This type of anxiety is counter-productive. In fact, studies show that patients with high anxiety have more problems navigating their way back to health.
Wellcome Images, Wikimedia Commons
An 1892 sketch of a woman in the midst of a panic attack.
How do we treat anxiety?
If you and your physician agree that you’re experiencing high and harmful levels of anxiety, then it makes sense to take steps to lower your anxiety. Often this can be done by changing your mindset and daily habits. When you feel a panic attack approaching, try to focus your mind on topics unrelated to your illness. Activities like gardening, reading and writing have all shown to lessen anxiety levels.
Often physical cues can bring about panic. Pain and shortness of breath are the two most common physical causes of anxiety in a palliative care scenario. By managing pain and getting more oxygen you could be eliminating a root cause of the problem.
In regards to traditional medication, patients are often prescribed benzodiazepines. This is a popular class of anxiety reducing drugs. Benzodiazepines act on the GABA receptors found on our brain cells. Our GABA brain cells are the part of our brain that calms us down. So it makes sense that a drug that enhances GABA would temper our anxiety. Common benzodiazepines include: Xanax, Ativan, Klonipan and Valium. The downside to these drugs is that they’re often psychologically addictive. This explains why they’re only recommended for 2-4 weeks. SSRI based anti-depressants (Paxil, Ativan, Prozac, ext.) and Buspirone are other prescription drugs used to treat anxiety.
Medicinal plants used to treat anxiety
Herbs have been used for centuries in traditional medicine to combat anxiety. Today, some of the commonly used botanical approaches to anxiety include: St. John’s wort, valerian, lavender and passionflower.
Valerian is sold as a supplement for a range of conditions including: insomnia, depression and anxiety. The valerian supplement is derived from the root of the Valerian plant (Valeriana officinalis). Evidence is mixed in regards to the effectiveness of valerian to treat anxiety. Some small studies demonstrate valerian can help reduce anxiety, while other studies find that valerian treatment is not better than a placebo treatment.
St. John’s wort is a yellow-flowered herb that grows well in temperate climates. The flowering heads of the plant have been used to treat depression and other health issues for many centuries. In general, St. John’s wort has shown to be effective for the treatment of mild to moderate depression. In addition, some reports suggest that taking St. John’s wort alone or in combination with valerian may improve anxiety disorder. However, more work is necessary to confirm this suggestion.
Passionflower (Passiflora incarnata) grows along vines and produces beautiful, intricate flowers. The flower can commonly be seen growing in southern United States. A few studies have shown that passionflower supplements can relieve anxiety as successfully as some benzodiazepines. For example, one small study, performed on 36 patients suffering from general anxiety disorder (GAD), demonstrated that passionflower was as effective as oxazepam. Oxazepam is a common prescription drug used to treat anxiety. More works needs to be done on passionflower and anxiety. The safety of long-term use has not been well established.
Lavender is a fragrant herb native to the Mediterranean region. Lavender has a long history of use as a medicinal plant. Historically, it has been used to boost appetite, mood and relieve anxiety. Many people are also fond of using lavender to help regulate their anxiety. However, there is very little evidence – at this moment – to support the use of lavender for most health issues, including anxiety. That said, one small study on healthy men has shown that an ingested lavender formula could reduce anxiety.
Return to our main list of symptoms.
Insomnia
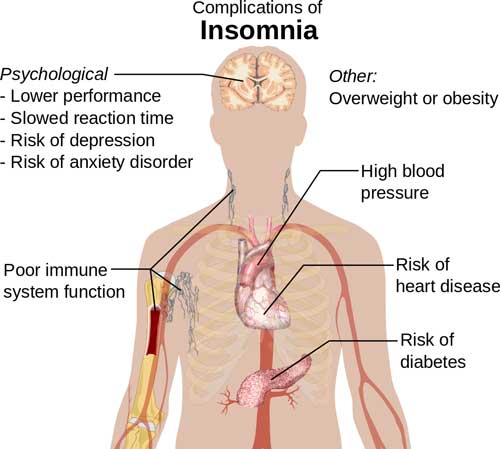
If you have persistent problems falling asleep and staying asleep, then you’re likely suffering from insomnia.
And – if you do suffer from this sleeping disorder then you’re well familiar with the consequences: irritability, low energy, mental fog and a depressed mood.
Insomnia is a double-edged sword, your nights are long and unsatisfying while your days are dull and flat. An insomniac friend of mine describes her days as a blur, as if her mind were covered in hazy clouds.
Unfortunately, insomnia is a very common complaint from patients in palliative care. In fact, 60% of patients negotiating a serious illness also suffer from insomnia.
Why is insomnia so prevalent in palliative care?
Pain and psychological issues are the most common causes for insomnia in palliative care. It’s very difficult to relax and sleep deeply when your body is managing chronic pain and discomfort.
High anxiety can keep you from falling asleep and often leads to nightmares, which can shake people from their sleep. Similarly, depression tends to wake people up early in the morning and lower the overall quality of sleep.
Other contributing factors to insomnia in palliative care include: cytokine levels, cortisol awakening response, coffee use, alcohol use and kidney stress.
Treating insomnia in palliative care.
The first line of defense against insomnia is an attempt to reduce or eliminate the underlying causes of your sleeplessness. If high anxiety is keeping you from getting a good night’s sleep, then you need to take steps to reduce your anxiety. If chronic pain is waking you up at night, then speak with your physician about changing your pain management therapy.
Cognitive behavioral therapy (CBT) is another effective strategy to combat insomnia. Interestingly, recent reports from the NIH reveal that CBT is as effective as sleeping pills for the short-term treatment of insomnia. However, it should be noted that CBT requires the patient to be very proactive. It’s much more work than simply taking a sleeping pill but it has shown to be effective and is worth considering. The focus of CBT is to change your sleep habits and the way you schedule and manage your sleep. Generally, if you’re engaged in CBT for insomnia – you need to make regular visits to a trained therapist. The therapist will help you create a series of sleep assessments. You’re often asked to keep a sleep diary.
Sleeping aids to help combat insomnia
Ambien is one of the most common prescription drugs for insomnia.
Herbal remedies are also worth considering. Patients in palliative care have reported success with valerian and melatonin.
Valerian has been used as a medicinal plant for a long time. This plant was initially described by Hippocrates, the Greek physician regarded as the father of medicine. Today, the roots of this plant are ground up, placed in a capsule and used for the treatment of insomnia, depression, anxiety, ext. Reports on the effectiveness of valerian to treat insomnia are inconsistent, however many people swear by it.
Melatonin is a natural hormone that is produced in our brain. The levels of melatonin activated in our brain changes throughout the day. Melatonin levels naturally rise in the evening and decrease in the morning. Interestingly, turning on a light in the evening can block melatonin production. People with sleep disorders often use melatonin supplements. Some clinical reports have demonstrated the effectiveness of melatonin to improve insomnia conditions.
Return to our main list of symptoms.
Weight loss
Cachexia is the official term for the loss of muscle mass brought about by a low metabolic state. Cachexia is an ancient Greek word meaning ‘bad things in your state of being‘. Hippocrates, the famous Greek physician, often used this term to diagnose his patients.
Weight loss is common among patients experiencing illnesses such as cancer, AIDS, heart failure, kidney disease and COPD. Loss of body mass is caused by a diminished appetite and the shift in metabolism that often accompanies a serious illness. When your body is fighting off a disease, there’s often a shift in the chemical signals moving around your immune system. These chemical signals are called cytokines. A cytokine shift can switch the body to a slower metabolic state. In this state, less food is necessary to maintain the activity of the body.
How do you treat weight loss?
First of all, you should make an effort to enjoy eating food. Prepare your favorite meals and focus on nutrient-dense foods. That said, its important to remember that you can not simply eat your way out of cachexia.
Palliative care weight loss is largely caused by a shift in metabolic activity, therefore, the single act of packing on more calories won’t reverse the symptoms.
For some patients, prescription drugs such as corticosteroids and megestrol have brought about significant improvement with cachexia. On a short-term time frame, corticosteroids can improve anorexia and weakness in cancer patients. Progestational drugs, like megestrol, demonstrate the ability to increase fat tissue, improve appetite and enhance the general well-being of patients with AIDS or late-stage cancer. The exact reason that corticosteroids and megestrol improves these symptoms remains unclear.
Alternative approach to treating treat weight loss
Various herbal and dietary supplements are commonly used to treat cachexia. First of all, the use of cannabinoids has certainly helped some patients regain their appetite and diminish nausea.
WebMD also lists the following supplements as possibly effective for the treatment of cachexia:
Adenosine
Adenosine is a naturally occurring chemical in our body. It forms part of the critical ATP molecule. ATP (adenosine tri-phosphate) delivers energy to our cells and helps regulate our metabolism. Use of adenosine may help reverse weight loss associated with cancer.
Fish oil
Fish oil can be administered with a fish oil supplement or simply by eating fish.
Medium-chain triglycerides (MCTs)
MCTs are fats that are partially man-made. They are generally formed by processing fats found in palm oil or coconut oil. MCTs can be given intravenously to reduce weight loss/muscle mass in critically ill patients.
Sidenote: When WebMD lists a supplement as possibly effective, it means that ‘reputable scientific references suggest that the product might work for a specific use … and at least one study (in humans) found that the product might be effective’.
Return to our main list of symptoms.
Radiation skin damage
Radiation is part of the standard treatment for many local or locally advanced cancers, such as head, neck and breast cancer. More than half of cancer patients will receive radiation from an external-beam, ionizing-radiation machine. Unfortunately radiation treatment can lead to significant side effects, particularly skin damage, skin burn and inflammation. This side effect is called dermatitis.
Radiation therapy usually lasts for 6-7 weeks and radiation dermatitis typically begins half way into radiation therapy. This skin damage often produces a mild rash and itchy, peeling skin. A more severe reaction will include blisters and wet peeling skin. The head, neck and breast are sensitive areas, so radiation burn to these places can be particularly distressing. The sensation is similar to a very severe sunburn. Radiation dermatitis can definitely affect a patients’ quality of life.
Relief from this condition primarily involves the use of topical therapy such as lotion, ointments and salves. Below are some examples of botanical-based methods that may offer some benefit, as shown in clinical research studies.
Botanical-based creams for radiation dermatitis
A sandalwood and turmeric based topical cream has shown, in a pilot clinical study, to reduce the development of radiation dermatitis. Here you can find a similar turmeric skin cream.
Curcumin is the main biologically active ingredient in turmeric. Another clinical study demonstrated that oral intake of curcumin (up to 6 grams daily) during radiation therapy reduced the severity of radiation dermatitis in breast cancer patients. This study was a randomized, double-blind clinical trial.
St. John’s wort (Hypericum perforatum) and neem oil also reduced skin toxicity from head and neck radiation in a separate clinical study. This study was a single arm observational study. You can read this study in more detail here.
Melatonin has also demonstrated effectiveness in treating radiation dermatitis. A published report shows how a melatonin-based cream can help reduce dermatitis caused by breast radiation. This particular report was a phase II double-blind, randomized controlled trial.
In the past, aloe ointment was commonly used for radiation dermatitis. However, a recent phase III clinical trial, performed in 2015, showed that there was no significant benefit in aloe ointment therapy. In fact, the aloe ointment treatment produced a response that was comparable to simply keeping your skin dry with powder.
Return to our main list of symptoms.
Gas and bloating
Nobody wants to walk around with gas and a bloated abdomen. Unfortunately, certain diseases often lead to these unpleasant stomach conditions. Colon cancer and ovarian cancer can both cause gas and a bloated abdomen and pelvis area.
Women need to be especially cautious if they feel abdominal bloating. A brief, monthly period of feeling bloated may simply be associated with a menstrual cycle. However, women need to monitor this discomfort. If a painful or bloated feeling lasts for more than a few weeks, the cause cause could be ovarian cancer. Ovarian cancer can create a persistent and painful feeling in the pelvic and abdominal region.
Colon cancer can sometimes produce a tumor somewhere in the lower digestive tract. This tumor could cause a slight obstruction to gas and fluids, which would likely result in persistent and unpleasant gas and bloating.
How do you reduce gas and bloating?
Nobody wants to deal with persistent gas and bloating. Managing your illness is enough of a struggle, you don’t want to suffer through indigestion as well.
Probiotics seem to be an effective strategy to help manage these symptoms. Under normal circumstances, our gut is populated with lots of micro-organisms. This is normal. Most of these microbes are friendly bacteria that help us digest food. By adding more friendly, healthy bacteria to your gut, you often improve your overall digestion. Two of the most studied probiotic bacteria species are Lactobacillus acidophilus and Bifidobacterium lactis. Probiotic foods contain those bacteria and other friendly bacteria.
Here are some classic probiotic foods you can find in most grocery stores.
- pickles
- kimchi
- tempeh
- yogurt
- miso
Probiotics are also available as a dietary supplement. Depending on your eating preferences, a capsule based supplement could be an easier and more consistent way to maintain healthy gut flora.
In addition, the ginger plant can also be used to break up and release gas. It seems that ginger can also help speed up digestion. This means your stomach will empty and any residual gas will eventually be released out of your lower digestive tract.
Return to our main list of symptoms.
Hot Flash
Hot flashes are temporary moments of warm skin, intense body heat and sweating.
These flashes can be very uncomfortable and are often followed with a lowered body temperature, chills and shivering. The complete biological cause is not fully understood. However, we do know that our sex hormones do have an effect on our body temperature. For example, as women transition into menopause, their estrogen levels change and this can lead to hot flashes. Some evidence suggests that wearing tight clothes, feeling stressed and consuming alcohol, spicy foods or caffeine can also trigger a hot flash.
Hot flashes are common in cancer care and other palliative care scenarios. We know that treatments for breast cancer and prostate cancer lead to hormonal changes that can induce severe hot flashes. Specifically, breast cancer treatments that include tamoxifen or aromatase inhibitors can cause a hot flash reaction. In fact, 80% of women receiving tamoxifen report hot flashes. In men, testicle removal surgery or hormonal therapy (androgen, GRH, estrogen) leads to hot flashes.
How do you manage hot flashes?
Some patients are eligible for estrogen-replacement therapy. This treatment can eliminate hot flashes, however many cancer treatment plans will not allow for estrogen-replacement. Other conventional hot flash treatments include anti-depressants, anti-convulsants, clonidine and megestrol.
Patients that maintain a journal of their hot flash patterns can often figure out their triggers. If you document the severity and duration of your hot flash episodes you should be able to connect the symptom with the daily habits that caused it. Some patients have found that hot showers, hot weather and smoking cigarettes are hot flash triggers.
Other patients have reported improvement in regards to hot flash severity after practicing hypnotherapy and mindfulness meditation. Research on these lifestyle practices is only preliminary, but some studies have had promising results. In contrast, acupuncture does not seem to help.
Many natural products have been studied for menopause symptoms. However, there is no herbal supplement or dietary change has clearly shown to be helpful for hot flash symptoms.
Some people have reported that increasing phyto-estrogens in their diet (soy, flax-seed, ext.) has helped with hot flash symptoms. However, we are not aware of any clinical trials to support that claim.
Likewise, some people use Black Cohosh, DHEA and Dong Quai to help with hot flashes, however the data is very mixed in terms of the effectiveness of these supplements for this particular application.
A few studies suggest Vitamin E and omega-3 fatty acids (EPA from fish oil) can help reduce the severity of hot flash symptoms. For example, in one study, women taking vitamin E averaged one fewer hot flash per day.
Return to our main list of symptoms.
Neuropathy
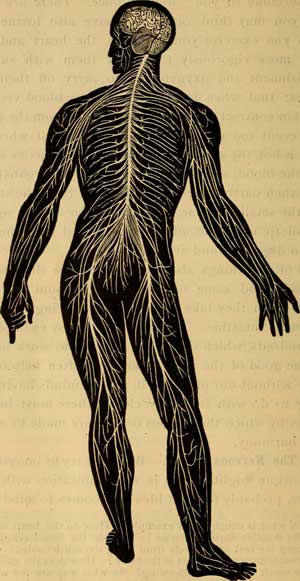
Neuropathy, also known as peripheral neuropathy, occurs when your peripheral nerves becomes damaged. The peripheral nerves are the intricate network of neurons that connect your brain and spinal cord to the rest of your body (skin, muscles, organs). When these nerves become damaged, a person will often feel numbness, pain, weakness, or a pins and needles sensation in some part of their body. Hands and feet are commonly affected by peripheral neuropathy.
Diabetes, shingles, auto-immune diseases, kidney failure or cancer treatment can often lead to some form of neuropathy.
Cancer patients often experience neuropathy as a side effect of receiving chemotherapy.
How do you treat neuropathy?
Ideally, the patient and physician can identify the root cause of the peripheral neuropathy. If that’s possible, then you can possibly design a strategy to eliminate the root cause. If you can’t eliminate the root cause, physicians will often prescribe an anti-depressant (amitriptyline), an anti-seizure drug or an opioid-based pain medication (oxycodone) in an attempt to reduce the effects of neuropathy.
Neuropathy affects our peripheral nervous system.
Alternative treatment for neuropathy
Herbal remedies for neuropathy include capsaicin and primrose oil.
Capsaicin is the spicy substance found in hot peppers. You can apply a capsaicin based cream to the affected areas on your body. There may be a slight burning sensation when you apply the capsaicin cream, but this should lessen over time.
Evening primrose oil has also shown the ability to reduce neuropathy pain among diabetics.
In addition, some chemotherapy patients report improvements upon using acetyl-L-carnitine, an amino acid supplement.
Return to our main list of symptoms.
Edema
Edema is the swelling of fluids in the body. Patients undergoing treatment for serious illness often experience swelling of the extremities. This means that the feet, legs and hands swell up because fluid builds in the body. When swelling occurs in the legs, this is referred to as peripheral edema. Edema is often caused by some problem in either the circulatory system, lymphatic system or kidneys.
Edema is common in cancer patients. This symptom is especially prevalent in kidney, liver and ovarian cancer. Chemotherapy, a common treatment for cancer, can also lead to swelling. Cisplatin and docetaxel are both chemotherapy drugs that can result in edema. Occasionally, other medications will cause body swelling, such as corticosteroids, NSAID pain-kilers and hormone replacement drugs.
How do you reduce this unpleasant swelling?
Ideally, you and your physician can identify the root cause of the fluid buildup. If one particular medication is causing edema, then hopefully you can find a suitable substitute.
Your physician may also be able to recommend a prescription diuretic. A diuretic drug should help rid your body of extra fluid.
In terms of lifestyle changes, often a small change to your diet can make a big difference. In general, a healthy and low-salt diet helps reduce swelling. The use of compression socks are also helpful for some folks suffering from peripheral edema.
A healthy heart can also minimize the effects of edema. A robust heartbeat helps push fluids around your body. This will keep fluids from pooling up in the extremities of your body. You can keep your heart pumping by maintaining a regular routine of daily exercise.
You can also explore the option of herbal diuretics. Certain plants help reduce body fluid levels. However, it’s also possible to lose vitamins and minerals with diuretics, so take caution and talk to your provider before trying a herbal diuretic.
The dandelion plant (Taraxacum officinale) is used as a herbal diuretic. But be aware, this plant may also interact with other medications (blood thinners, antibiotics, lithium, ext.)
Grape seed extract and bilberry are two additional botanical sources regarded as useful for edema.
Return to our main list of symptoms.
Urinary health
On occasion, the urinary tract can become infected, leading to a urinary tract infection (UTI). This symptom mostly affects women and older men. Patients that are negotiating neurological disorders, such as Parkinson’s or Alzheimers, can also develop UTIs.
Any scenario where you are not completely emptying your bladder can potentially lead to an UTI. If urine is pooled up in your bladder, eventually bacteria will begin to grow in the stagnant fluid. An enlarged prostate, diminished muscle strength around the bladder, lack of estrogen in women and a weakened immune system can all contribute to an improperly functioning bladder, which can then lead to an UTI. Each year, there is a staggering 8 million doctor visits that are related to UTIs.
How do you maintain urinary health?
Antibiotics are often the first line of defense against UTIs, especially when severe symptoms are present. However, antibiotics are not the only treatment option.
First of all, make sure you are drinking lots of water. Water flushes out your system and this will help clean out your urinary tract.
In addition, maintain a diet that is high in Vitamin C. High levels of Vitamin C will raise the acidity of your urine. Most bacteria do not like an acidic environment and so this will limit their growth.
Medicinal plants used to treat urinary tract infections
Herbs that are effectively used to maintain urinary health include: bearberry leaf and goldenseal.
Bearberry leaf (Arctostaphylos Uva-Ursi) is a small, bushy plant that grows in the northern latitudes. This plant is often used in response to lower urinary tract infections.
The goldenseal plant contains a chemical called berberine. Berberine helps fend off bacteria populations. Reports have shown that berberine is effective at limiting E.coli bacteria from binding to the walls of the urinary tract.
Return to our main list of symptoms.
Dry mouth
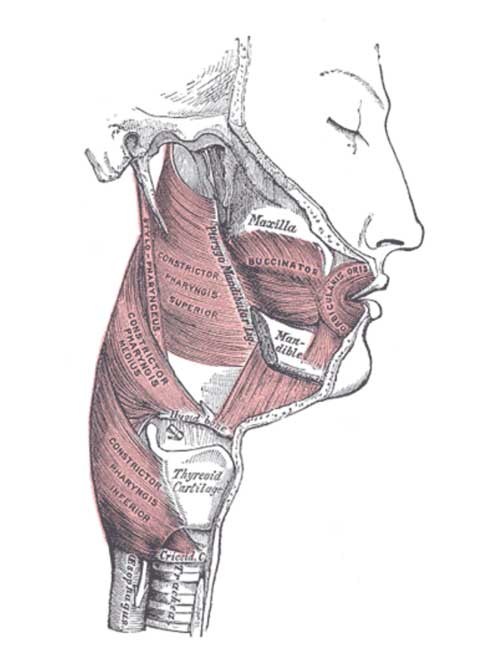
Its easy to take a moist mouth for granted, until it’s gone. Dry mouth, also known as xerostomia, occurs when your salivary glands don’t generate enough saliva to keep your mouth wet. If you suffer from this dry mouth condition, you may have trouble chewing food, swallowing, tasting flavors and even talking. In addition, dry mouth can lead to more severe mouth problems. Our saliva helps regulate the bacteria populations in our mouth. When our mouth becomes dry, our mouth bacteria may over-populate and create infections that can lead to gum disease and cavities. In summary, you want to do your best to avoid dry mouth.
Unfortunately, cancer treatments such as chemotherapy and radiation can damage your salivary glands and cause this dry mouth symptom. Other medical scenarios that lead to dry mouth include: diuretic medication, use of anti-depressants, tissue/organ transplants and the use of certain painkillers.
How do you treat dry mouth?
If you cannot terminate the treatment that is causing your dry mouth, then the best you can do is manage the symptom. Prescription medicines such as Salagen and Evoxac can stimulate your salivary glands to produce more spit. You can also use a mouth rinse that acts as a substitute for saliva, such as carmellose or hyprolose. Chewing sugarless gum is another simple trick that can keep your mouth moist.
In order to minimize other mouth issues while you negotiate your dry mouth symptom, you should do your best to maintain dental hygiene. Brush after each meal with a soft toothbrush, rinse your mouth with salt and baking soda 5-7 times daily, drink lots of water, avoid mouthwashes with alcohol. Visit your dentist for more advice.
Cayenne pepper and fennel seeds are two botanical sources used to treat dry mouth. These are cheap and simple home remedies that help increase saliva in your mouth.
Some people take a pinch of ground cayenne pepper and simply rub it around their mouth and tongue. Or you can use cayenne as a seasoning with your meals; the pepper adds a spicy flavor to any salad, soup or meat dish.
Fennel seeds are commonly chewed after a meal to cleanse the palette and freshen one’s breath. You often see a bowl of fennel seeds near the cash register at Indian restaurants. Fennel seeds are also used to reduce dry mouth. There are flavonoids in fennel seeds that can help stimulate the flow of saliva in your mouth. Give it a try!
Return to our main list of symptoms.
Mucositis
Mucositis occurs when the mucous membranes lining our digestive and respiratory tracts become infected and inflamed. Once the lining of the digestive and respiratory tracts becomes damaged, the effects of mucositis can follow:
- Red, swollen mouth and gums
- Weight loss
- Taste change
- Blood in the mouth
- Difficulty swallowing or talking
- Pain in the mouth and throat
- Increased mucus or thicker saliva
This inflammation and ulceration of body tissue often happens as a side effect of chemotherapy and radiation treatments. Mucositits is an especially big problem for patients who receive radiation in the head and neck areas. These cancer treatments are destructive to the surface cells of these sensitive body tissues. While you are suffering from mucositis, the focus should be on the palliation, or reduction, of symptoms. Once the cancer treatment is finished, your mouth should heal itself gradually.
Patients dealing with kidney disease, diabetes or HIV/AIDS also suffer from mucositis.
How do you treat mucositis?
First of all, you want to keep this damaged tissue clean. Frequent rinsing with an anti-septic mouth wash will help. You can try Peridex or Periogard. You can also create your own mouth rinse. Mix up 8 ounces of water and 1 teaspoon of baking soda. This rinse will help keep your throat clean.
To counter the effects of a dry mouth, try chewing on ice chips or chewing on sugar-free gum.
If sores in your mouth and throat become infected – you can gargle with a homemade cleaning solution. Mix up 1 cup of 3% hydrogen peroxide with 1/2 teaspoon of salt and 2 cups of water. Do NOT swallow this mixture. Gargle and spit it out.
The pain and discomfort of mucositis can be managed by chewing ice chips to numb the mouth. If you need stronger pain relief, consider a topical pain remedy (lidocaine,benzocaine, ext.)
Pure natural honey is another great remedy for mucositis. Thick, viscous honey creates a protective barrier around the sensitive tissues in the throat and mouth. Honey also has natural anti-bacterial properties, this helps defend against infection. Here is a study that demonstrates honey can significantly improve mucositis conditions and can also reduce the risk of yeast and bacteria infection. Thanks honey bees!
Mouthwashes can be prepared with other herbs. In general herbal mouthwashes are safe and easy to prepare. We will list some herbs that have demonstrated effectiveness in published clinical trials. Click on each herb to read more details on their respective clinical trial.
- Common Yarrow
- Aloe vera
- Chamomile
- Chamomile plus peppermint
- Turmeric
- Indigowood root
- Coffee plus honey
- Samital
A personal note from Walter Tsang MD: I have recommended people dealing with mucositis to try chamomile tea mouthwash (with and without honey) and these patients thought it helped.
Return to our main list of symptoms.
This concludes our list of health issues associated with palliative care.
The list is a work in progress, so please bookmark the page and return often.
I’ll be updating the page each year as new research is published on effective integrative therapies.
Thanks for stopping by!
References
(Most of the key references for this article are linked within the text. Below we list some additional sources for each section.)
Fatigue
Radbruch, Lukas, et al. “Fatigue in palliative care patients—an EAPC approach.” Palliative Medicine 22.1 (2008): 13-32.
Escalante, Carmen P. “Treatment of cancer-related fatigue: an update.” Supportive care in cancer 11.2 (2003): 79-83.
Nausea
Glare, Paul, et al. “Treating nausea and vomiting in palliative care: a review.” Clin Interv Aging 6.243 (2011): 59.
Loss of appetite
Davis MP, Walsh D, Lagman R, Yavuzsen T. Early satiety in cancer patients: a common and important but underrecognized symptom. Support Care Cancer, 2006 Jul;14(7):693-8. Epub 2006 Apr 20.
Hovan AJ, Williams PM, Stevenson-Moore P, Wahlin YB, Ohrn KE, Elting LS, et al. A systematic review of dysgeusia induced by cancer therapies. Support Care Cancer 2010;18(8):1081-7. Epub 2010 May 22.
Cognitive decline
Ostgathe, Christoph, Jan Gaertner, and Raymond Voltz. “Cognitive failure in end of life.” Current opinion in supportive and palliative care 2.3 (2008): 187-191.
Radiation dermatitis
Rao, Suresh, et al. “The Indian spice turmeric delays and mitigates radiation-induced oral mucositis in patients undergoing treatment for head and neck cancer: an investigational study.” Integrative cancer therapies 13.3 (2014): 201-210.
Franco, Pierfrancesco, et al. “Hypericum perforatum and neem oil for the management of acute skin toxicity in head and neck cancer patients undergoing radiation or chemo-radiation: a single-arm prospective observational study.” Radiation Oncology 9.1 (2014): 297.
Ryan, Julie L., et al. “Curcumin for radiation dermatitis: a randomized, double-blind, placebo-controlled clinical trial of thirty breast cancer patients.” Radiation research 180.1 (2013): 34-43.
Ben-David, Merav A., et al. “Melatonin for Prevention of Breast Radiation Dermatitis: A Phase II, Prospective, Double-Blind Randomized Trial.” The Israel Medical Association journal: IMAJ 18.3-4 (2015): 188-192.
Hoopfer, Donna, et al. “Three-arm randomized phase III trial: quality aloe and placebo cream versus powder as skin treatment during breast cancer radiation therapy.” Clinical breast cancer 15.3 (2015): 181-190.
Anxiety
Chochinov, Harvey Max, and William Breitbart. Handbook of psychiatry in palliative medicine. Oxford University Press, USA, 2009.
Curran, Kevin P., and Sreekanth H. Chalasani. “Serotonin circuits and anxiety: what can invertebrates teach us?.” Invertebrate Neuroscience 12.2 (2012): 81-92.
Depression
Marks, Sean, and Thomas Heinrich. “Assessing and treating depression in palliative care patients.” Current Psychiatry 12.8 (2013): 35.
Wilson, Keith G., et al. “Diagnosis and management of depression in palliative care.” Handbook of psychiatry in palliative medicine (2000): 25-49.
Insomnia
Renom-Guiteras, Anna, et al. “Insomnia among patients with advanced disease during admission in a Palliative Care Unit: a prospective observational study on its frequency and association with psychological, physical and environmental factors.” BMC palliative care 13.1 (2014): 1.
National Institutes of Health. “National Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults, June 13-15, 2005.” Sleep 28.9 (2005): 1049.
Hot Flashes
Boekhout, Annelies H., Jos H. Beijnen, and Jan HM Schellens. “Symptoms and treatment in cancer therapy-induced early menopause.” The oncologist 11.6 (2006): 64.
Cachexia
Bruera, Eduardo. “ABC of palliative care. Anorexia, cachexia, and nutrition.” BMJ: British Medical Journal 315.7117 (1997): 1219.
Gas and bloating
Ringel, Yehuda, et al. “T1406 Probiotic Bacteria Lactobacillus Acidophilus Ncfm and Bifidobacterium Lactis Bi-07 Improve Symptoms of Bloating in Patients with Functional Bowel Disorders (FBD).” Gastroenterology 134.4 (2008): A-549.